The Detrimental Ripple: Unpacking the Negative Impacts of New Medicaid Work Requirements
Executive Summary
The proposed reintroduction and expansion of Medicaid work requirements represent a significant shift in health policy, ostensibly aimed at promoting employment and reducing healthcare expenditures. However, a comprehensive examination of historical implementations and projected impacts reveals a starkly different reality. This report synthesizes extensive research to demonstrate that these restrictions are empirically proven to lead to substantial coverage losses, disproportionately burdening vulnerable populations, escalating emergency room utilization, and increasing overall healthcare costs across the system. Far from achieving their stated objectives, Medicaid work requirements function primarily as a mechanism for disenrollment, imposing significant administrative and financial strains on individuals, healthcare providers, and state economies, ultimately undermining the very foundations of public health and economic stability.
Introduction: The Resurgence of Medicaid Work Requirements – A Policy Re-examined
For the majority of its history, Medicaid, the vital joint state and federal health insurance program for individuals with low incomes, has not linked eligibility to employment status (Commonwealth Fund, 2025a; Health Management, 2025a). This long-standing policy began to change during the first Trump administration, which actively encouraged state Medicaid agencies to experiment with work requirements through Section 1115 waivers (Commonwealth Fund, 2025a; Health Management, 2025a). Between 2017 and 2021, eleven state proposals received federal approval for these demonstration programs. Nevertheless, most of these initiatives never fully materialized due to a combination of legal challenges and the widespread economic disruption brought on by the COVID-19 pandemic (Commonwealth Fund, 2025a). The subsequent Biden administration then rescinded approval for all such proposals in early 2021 (Commonwealth Fund, 2025a).
Despite these past setbacks, the landscape of Medicaid policy is poised for a significant shift once again. Under a new Trump administration, the concept of Medicaid work requirements is expected to experience a resurgence (Commonwealth Fund, 2025a; Health Management, 2025a). This is underscored by recent legislative efforts, notably the "One Big Beautiful Bill Act" (H.R. 1) advanced by the U.S. House of Representatives, which includes a nationwide work and community engagement requirement with an ambitious implementation deadline of December 31, 2026 (CBS News, 2025; Health Management, 2025a). These requirements typically mandate that working-age Medicaid beneficiaries, generally those between the ages of 18 and 64, demonstrate a minimum of 80 hours per month, or 20 hours per week, of employment, volunteering, or engagement in educational activities to maintain their health coverage (Commonwealth Fund, 2025a; Health Management, 2025a).
Historically, only two states have fully implemented Medicaid work requirements. Arkansas was the first, launching its program in June 2018, only for it to be terminated by a court order in March 2019 (Ballotpedia, n.d.; Commonwealth Fund, 2025a; National Health Law Program, 2025). More recently, Georgia implemented its Pathways to Coverage program in July 2023, which incrementally expands Medicaid eligibility contingent upon meeting a work reporting requirement (Ballotpedia, n.d.; Commonwealth Fund, 2025a).
Proponents of these policies frequently assert that work requirements serve to encourage employment, foster self-sufficiency, and reduce overall healthcare spending (CBS News, 2025; Fierce Healthcare, 2025; Robert Wood Johnson Foundation, 2025). For instance, the Congressional Budget Office (CBO) projected that the work requirements within the House bill could reduce spending by $344 billion (Fierce Healthcare, 2025). However, a substantial body of research and findings from previous Medicaid work requirement initiatives consistently contradicts these optimistic claims (ACLU, 2025; Brookings, 2025a; Center on Budget and Policy Priorities, 2025a; Commonwealth Fund, 2018; Commonwealth Fund, 2025b; National Health Law Program, 2025; Robert Wood Johnson Foundation, 2025; Urban Institute, 2025). In fact, the CBO itself concluded that Medicaid work requirements would "have a negligible effect on employment status or hours worked by people who would be subject to the work requirements" (Commonwealth Fund, 2025b; Commonwealth Fund, 2025c). This fundamental disparity between the stated policy intent and the observed empirical outcomes highlights a critical misjudgment. The policy's underlying assumption that Medicaid disincentivizes work appears to be deeply flawed when examined against the real-world circumstances of beneficiaries. Consequently, if the primary goals of increasing employment and achieving cost savings are not met, the policy's true and most significant effect becomes coverage loss, effectively transforming it into a de facto mechanism for reducing Medicaid enrollment rather than genuinely promoting self-sufficiency. This raises profound questions about the true motivations behind such policies and the ethical implications of implementing measures known to fail their stated objectives while simultaneously causing demonstrable harm.
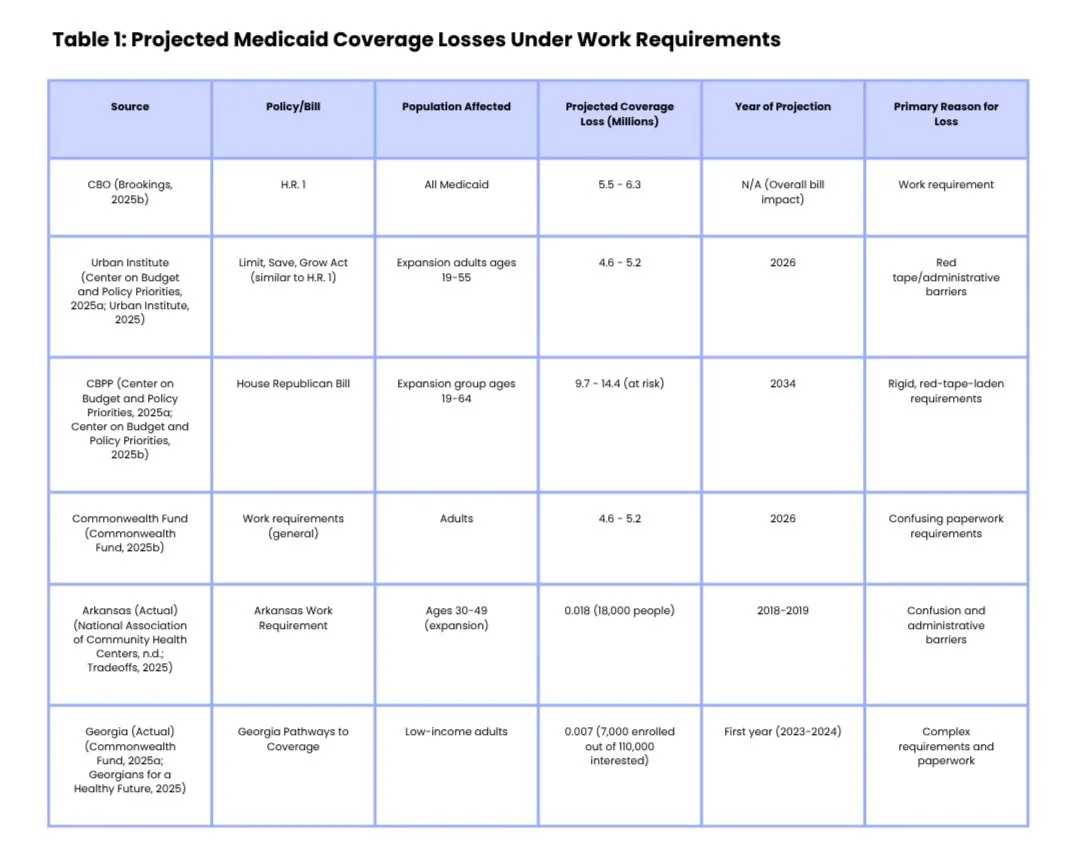
Erosion of Health Coverage and Disproportionate Harm to Vulnerable Populations
The reintroduction of Medicaid work requirements is projected to lead to a significant reduction in health coverage, primarily due to the complex administrative hurdles imposed on beneficiaries. The House bill, for example, is projected to result in approximately 11 million people becoming uninsured, with 5.5 to 6.3 million losing Medicaid coverage specifically because of work requirements (Brookings, 2025b; Center on Budget and Policy Priorities, 2025a). Other analyses from the Urban Institute and Brookings Institution estimate coverage losses ranging from 4.6 million to 5.2 million by 2026 (Center on Budget and Policy Priorities, 2025a; Commonwealth Fund, 2025b; Urban Institute, 2025). Looking further ahead, the Center on Budget and Policy Priorities estimates that between 9.7 million and 14.4 million individuals could be at risk of losing Medicaid coverage by 2034 under the proposed House Republican bill (Center on Budget and Policy Priorities, 2025a; Center on Budget and Policy Priorities, 2025b).
A critical finding from past implementations is that a substantial portion of coverage loss occurs not because individuals are unwilling or unable to work, but rather due to overwhelming "red tape" and administrative barriers (ACLU, 2025; Center on Budget and Policy Priorities, 2025a; Center on Budget and Policy Priorities, 2025b; Commonwealth Fund, 2025b; Georgians for a Healthy Future, 2025; Health Management, 2025a; National Association of Community Health Centers, n.d.; National Health Law Program, 2025; Robert Wood Johnson Foundation, 2025). The experience in Arkansas, the first state to fully implement these requirements, serves as a stark illustration. Over 18,000 people, representing 28% of the target population, lost Medicaid coverage primarily because of confusion and administrative hurdles (ACLU, 2025; Milbank Memorial Fund, 2025; National Association of Community Health Centers, n.d.; Tradeoffs, 2025; Urban Institute, 2025). Similarly, in Georgia’s Pathways to Coverage program, out of 110,000 individuals who expressed interest in applying during the first year, only about 5%, or 7,000 people, successfully navigated the complex application process and enrolled (Commonwealth Fund, 2025a; Georgians for a Healthy Future, 2025). The Urban Institute estimated that while over 90% of working-age adults enrolled in Medicaid either work or would qualify for an exemption, between 36% and 42% could still lose coverage simply due to the complexities of reporting (Commonwealth Fund, 2025d; Robert Wood Johnson Foundation, 2025). For populations heavily reliant on manual reporting, this risk of coverage loss escalates dramatically to 72% (Commonwealth Fund, 2025d).
This phenomenon highlights that administrative burden serves as the primary mechanism of coverage loss. While work requirements often include exemptions for individuals with disabilities, chronic conditions, or caregiving responsibilities (CBS News, 2025; Center on Budget and Policy Priorities, 2025a; Center on Budget and Policy Priorities, 2025b; Health Management, 2025a; National Association of Community Health Centers, n.d.), and data indicates that most Medicaid recipients already work or fall into these exempt categories (ACLU, 2025; Brookings, 2025a; Commonwealth Fund, 2025b; KFF, 2025; Robert Wood Johnson Foundation, 2025), the observed outcome is still millions losing coverage due to procedural issues. This suggests that the policy's effect is not primarily about incentivizing work but rather about creating procedural hurdles that effectively disenroll eligible individuals. The administrative complexity, rather than a lack of work, becomes the driving force behind coverage loss. Consequently, any "savings" achieved through disenrollment are not a result of increased employment and self-sufficiency, but rather reduced access to necessary healthcare for a population that largely qualifies for it, effectively shifting the burden from federal and state budgets to individuals and the uncompensated care system, thereby undermining the very purpose of a safety-net program.
Work requirements disproportionately harm specific vulnerable groups, creating a "Catch-22" for the medically vulnerable. While exemptions are intended for people with disabilities, caregivers, and those with chronic conditions, these are precisely the individuals who struggle most to navigate complex reporting systems (ACLU, 2025; Bazelon Center for Mental Health Law, 2025; Center on Budget and Policy Priorities, 2025b; Commonwealth Fund, 2025d; National Association of Community Health Centers, n.d.; Robert Wood Johnson Foundation, 2025). The very conditions that qualify someone for an exemption, such as a chronic illness, disability, or caregiving demands, also make it significantly more difficult for them to comply with the administrative burden of proving their exemption or work status (ACLU, 2025; Bazelon Center for Mental Health Law, 2025; Commonwealth Fund, 2025d; Robert Wood Johnson Foundation, 2025). This administrative burden acts as a de facto barrier to care for those who need it most, exacerbating health disparities and potentially leading to worse health outcomes, further straining emergency services and uncompensated care. Medically frail individuals, defined as those with chronic, serious, or complex medical conditions, require identification and exemption, yet the process for doing so can be challenging (Health Management, 2025a; National Health Law Program, 2025). Community health centers (CHCs), which serve over 31 million people nationwide—often patients who are older, in poorer health, and facing significant health and social burdens—could see nearly 5.6 million of their patients lose coverage due to these requirements (Commonwealth Fund, 2025d).
The implications extend beyond individuals to families, particularly children, through what is known as the "welcome mat" effect. When parents have Medicaid coverage, their children are more likely to be insured (Center for American Progress, 2025). Medicaid work requirements threaten this crucial dynamic, as parents who lose coverage due to bureaucratic barriers can inadvertently cause their children to lose coverage as well, even if the children remain eligible (Center for American Progress, 2025). A May 2025 analysis projected that 480,000 children could lose coverage if work reporting requirements applied only to expansion adults, a number that could rise to 914,000 children if applied to all non-disabled adults (Center for American Progress, 2025). This means that the administrative burden placed on adults has a direct, negative, and unintended intergenerational consequence, undermining child health and well-being. This outcome contradicts public health goals of ensuring child health and could lead to long-term negative health and developmental outcomes for children, increasing future healthcare costs and societal burdens. It highlights how a policy seemingly targeting "able-bodied adults" has far-reaching effects on dependent populations.
Furthermore, the premise that work requirements lead to employment gains is a persistent myth, consistently disproven by evidence from past implementations. Research overwhelmingly shows that work requirements do not increase employment (ACLU, 2025; Brookings, 2025a; Center on Budget and Policy Priorities, 2025a; Commonwealth Fund, 2018; Commonwealth Fund, 2025b; National Health Law Program, 2025; Robert Wood Johnson Foundation, 2025; Urban Institute, 2025). Experiences with work requirements in other income support programs, such as Temporary Assistance for Needy Families (TANF) and the Supplemental Nutrition Assistance Program (SNAP), have yielded only mixed results, with slight employment gains but no increase in average income (Commonwealth Fund, 2025a; Commonwealth Fund, 2018). SNAP work requirements, in particular, have been shown to significantly reduce program participation by as much as 53% without corresponding employment effects (Brookings, 2025a; Robert Wood Johnson Foundation, 2025). In Arkansas, after 18 months of implementation, there was no measurable increase in employment, despite 18,000 people losing coverage (ACLU, 2025; Milbank Memorial Fund, 2025; Tradeoffs, 2025; Urban Institute, 2025). The vast majority of Medicaid enrollees who are able to work already do so, with 64% working full or part-time (KFF, 2025; Robert Wood Johnson Foundation, 2025). Most of those who do not work are typically caregivers (12%), ill or disabled (10%), or students (7%) (Commonwealth Fund, 2025b; Robert Wood Johnson Foundation, 2025). Only about 8% are not working or unable to find work for other reasons (Commonwealth Fund, 2025b). This consistent empirical reality demonstrates that the policy fundamentally misdiagnoses the reasons for non-employment among Medicaid beneficiaries. It attempts to solve a problem that largely does not exist for the target population, rendering the chosen solution of mandating work ineffective. This implies that the policy is not designed to support employment but rather to reduce program enrollment. Instead of addressing underlying barriers to employment—such as lack of job training, reliable transportation, or childcare support—it imposes punitive measures that remove health coverage, potentially making it even harder for individuals to maintain or seek employment due to poor health (Commonwealth Fund, 2025b; Commonwealth Fund, 2018).
Increased Emergency Department Utilization and Deterioration of Health Outcomes
The loss of Medicaid coverage due to work requirements is directly linked to a deterioration of health outcomes and an increased reliance on emergency services. Research consistently demonstrates that disruptions in Medicaid coverage, often referred to as "churning," frequently lead to periods of uninsurance, delayed medical care, and reduced access to preventive services for beneficiaries (ASPE, n.d.). Individuals who experience even short periods of uninsurance, such as 1 to 5 months, exhibit worse access to care compared to those with continuous coverage throughout the year (ASPE, n.d.). When millions of people lose Medicaid coverage, they are effectively cut off from essential services, including access to necessary medications, routine doctor visits, and critical treatments (ACLU, 2025). This creates a preventable health crisis, where treatable conditions are left unaddressed or worsen, ultimately leading to more severe health crises that necessitate more intensive and expensive interventions. The supposed "savings" derived from disenrollment are thus offset by the higher costs associated with managing neglected health issues. This undermines the public health goal of promoting wellness and early intervention, shifting the point of care from primary and preventive settings to acute, crisis-driven environments, which ultimately leads to poorer population health outcomes and increased suffering.
The evidence of increased emergency room (ER) visits and hospitalizations following coverage gaps is compelling. Studies indicate that beneficiaries who churn in and out of Medicaid coverage experience higher monthly healthcare costs due to pent-up demand for health services (ASPE, n.d.). One study specifically found that unstable Medicaid coverage resulted in a 10% to 36% increase in emergency department use, office visits, and hospitalizations (ASPE, n.d.). Furthermore, interruptions in coverage can lead to a rise in emergency room visits, hospitalizations, and admissions to psychiatric facilities, potentially pushing individuals with mental health disabilities into institutional settings (Bazelon Center for Mental Health Law, 2025). Data from Texas illustrates this point, reporting approximately 1.6 million potentially preventable emergency room visits in Medicaid and CHIP in 2023, with associated expenditures of $754 million in 2022 (Texas Health and Human Services, 2024; Texas Health and Human Services, 2025). These were visits that "could have been managed in physician offices or clinics" (Texas Health and Human Services, 2024; Texas Health and Human Services, 2025). This represents a significant "cost shifting" to emergency care. When primary care becomes inaccessible due to coverage loss, individuals with urgent or worsening conditions are compelled to resort to the emergency department, a setting designed for acute care, not routine health management. This results in an increase in preventable ER visits, as evidenced by the Texas data, where the "savings" from disenrollment are effectively negated by higher, less efficient costs incurred in the ER setting. This not only inflates healthcare costs but also places an undue strain on emergency departments, which are often already overburdened. It signifies a systemic failure to provide appropriate, timely care, forcing vulnerable individuals into a more expensive and less effective care pathway.
The impact on mental health and substance use disorder services is particularly concerning. A significant proportion of Medicaid beneficiaries utilize mental health and substance use services (Brookings, 2025b). Withdrawing care from this population, as work requirements are prone to do, will undoubtedly cause harm and is highly unlikely to promote community engagement (Brookings, 2025b). Imposing work requirements would severely impact people with mental health disabilities, creating additional barriers to their employment, stripping them of healthcare coverage, and denying them the necessary services and supports to thrive (Bazelon Center for Mental Health Law, 2025). This will lead to untreated or undertreated conditions, an increase in crises, and a greater likelihood of reliance on emergency services or even institutionalization for mental health issues (Bazelon Center for Mental Health Law, 2025). The policy, while ostensibly promoting work, actively undermines the health stability necessary for employment. This creates a public health crisis for a highly vulnerable population, increasing societal costs associated with untreated mental illness and substance use disorders, including homelessness, incarceration, and reduced productivity. It represents a significant step backward in addressing the opioid crisis and broader mental health epidemic.
Escalating Healthcare Costs Across the System
Beyond the direct impact on individuals and ER utilization, Medicaid work requirements introduce significant financial burdens across the entire healthcare system, often under the illusion of achieving savings.
High Administrative Burdens and Costs of Implementation
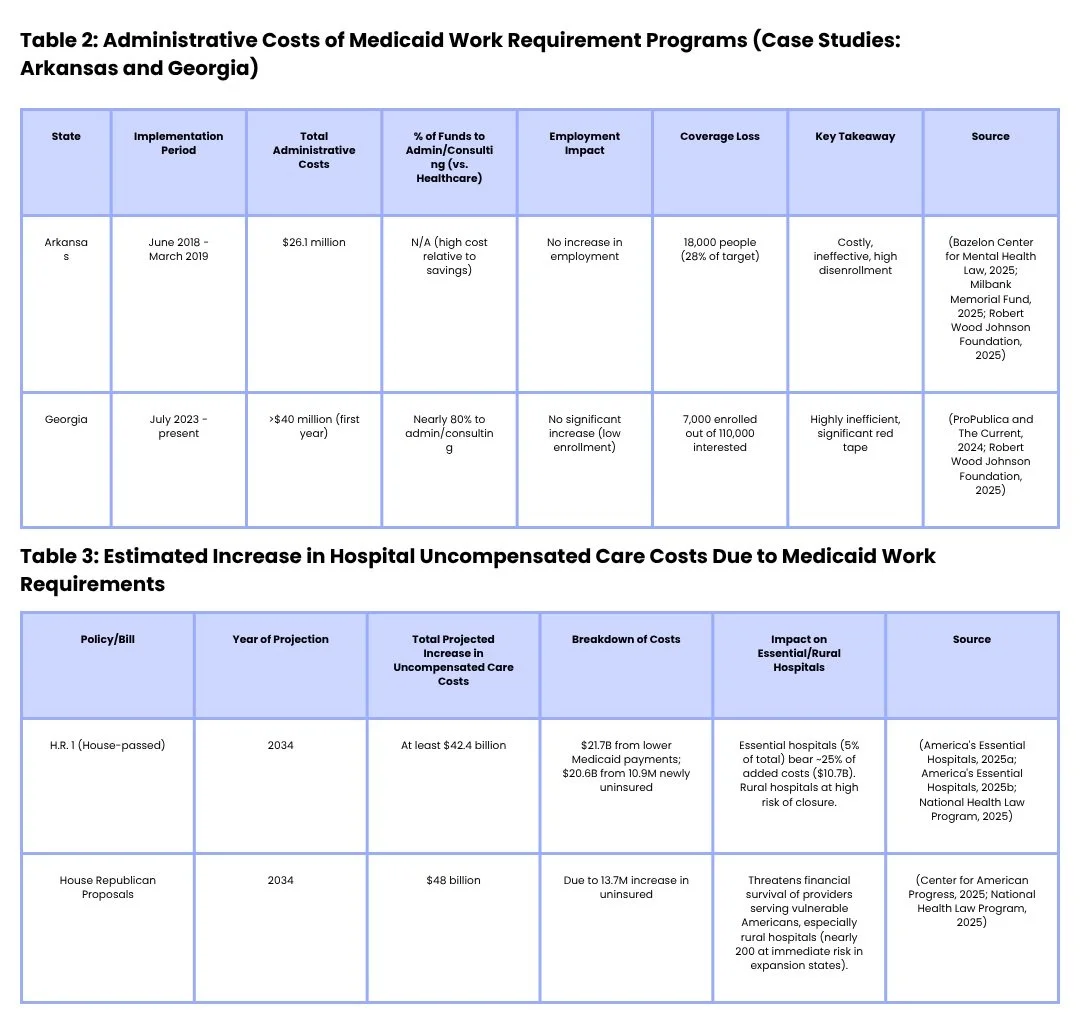
Implementing Medicaid work requirements is characterized by high administrative costs that often outweigh any potential savings (Health Management, 2025a; Health Management, 2025b). The experience of Arkansas demonstrates this clearly, with the state spending $26.1 million on its implementation without any corresponding increase in employment (Bazelon Center for Mental Health Law, 2025; Milbank Memorial Fund, 2025; Robert Wood Johnson Foundation, 2025). Georgia’s Medicaid program with work requirements incurred over $40 million in its first year, with nearly 80% of these funds being allocated to administrative and consulting fees rather than direct healthcare services (ProPublica and The Current, 2024; Robert Wood Johnson Foundation, 2025). States face the complex and costly task of developing and streamlining new systems for logging compliance activities, processing exemptions, and managing appeals (Health Management, 2025a; Health Management, 2025b). This creates an illusion of savings through administrative inefficiency. The "savings" projected by disenrollment are significantly eroded, or even outweighed, by the substantial cost of administering the requirements. This suggests that the policy is administratively inefficient and fiscally unsound if its goal is genuine cost reduction. This represents a misallocation of taxpayer funds, as money that could be spent on direct healthcare services, preventive care, or actual employment support programs is instead consumed by bureaucratic overhead, demonstrating a policy that is not only ineffective but also wasteful.
Increased Uncompensated Care for Hospitals and Providers
A major consequence of Medicaid work requirements is a substantial increase in uncompensated care costs for hospitals and other healthcare providers, particularly safety-net and rural facilities. The proposed Medicaid policy changes within H.R. 1 are projected to increase hospital uncompensated care costs by at least $42.4 billion in 2034 (America's Essential Hospitals, 2025a; America's Essential Hospitals, 2025b; National Health Law Program, 2025). This increase is attributed to two main factors: $21.7 billion from lower Medicaid payments and an additional $20.6 billion from 10.9 million newly uninsured individuals (America's Essential Hospitals, 2025a; America's Essential Hospitals, 2025b; National Health Law Program, 2025). Essential hospitals, despite accounting for only 5% of hospitals nationally, are estimated to bear approximately 25% of these added unpaid costs, totaling an additional $10.7 billion by 2034 (America's Essential Hospitals, 2025a; America's Essential Hospitals, 2025b; National Health Law Program, 2025).
The loss of coverage directly impacts hospitals by reducing their revenue and increasing the burden of uncompensated care, leading to diminished operating margins (Commonwealth Fund, 2025e; Commonwealth Fund, 2025f; National Health Law Program, 2025). These adverse financial outcomes affect not only Medicaid patients but also the entire community served by these hospitals, as reduced revenues could force facilities to cut staff or eliminate essential services (Commonwealth Fund, 2025e; Commonwealth Fund, 2025f). Rural hospitals are especially vulnerable, with many already operating at a loss (46% nationwide), and some states facing the grim prospect of over 40% of their rural hospitals being at risk of closure (National Health Law Program, 2025). This highlights the hidden burden on the healthcare safety net. The policy effectively shifts financial responsibility from the federal and state governments to individual hospitals and the broader healthcare system. This undermines the financial stability of critical healthcare infrastructure, particularly in underserved areas, threatening access to care for entire communities. This could lead to widespread hospital closures, especially in rural areas, creating healthcare deserts and exacerbating existing health inequities. It demonstrates that "cost savings" at the federal level translate into significant financial strain and reduced access to care at the local level, ultimately harming the very communities the healthcare system is meant to serve.
Financial Strain on Community Health Centers and the Broader Healthcare Ecosystem
Community health centers (CHCs) form a critical part of the primary care safety net for vulnerable populations. The imposition of work requirements could lead to nearly 5.6 million CHC patients losing coverage, resulting in a staggering loss of up to $32 billion in health center revenue (Commonwealth Fund, 2025d). As millions of patients lose their Medicaid coverage, CHCs will face immense challenges in managing treatment for highly vulnerable patients with complex needs who can no longer afford care, simultaneously struggling for their own economic survival (Commonwealth Fund, 2025d). This represents an undermining of the foundation of primary care for vulnerable populations. The financial viability of CHCs is directly threatened, potentially leading to reduced services, staff cuts, or even closures. This means that the primary care safety net for the most vulnerable populations is systematically weakened, forcing more individuals to rely on more expensive and less appropriate care settings, such as emergency rooms, further increasing overall healthcare costs and worsening health outcomes for those who lose access to their primary care providers. This highlights how policies aimed at reducing federal spending can dismantle crucial community-level health infrastructure.
Broader Economic Repercussions
The economic consequences of Medicaid work requirements extend far beyond the healthcare sector. Proposed requirements could lead to as much as $59 billion in lost state gross domestic products (GDPs) and the elimination of up to 449,000 jobs across multiple industries in 2026 alone (Center for American Progress, 2025; George Washington University, 2025). This includes a significant impact on the healthcare sector itself, with up to 206,000 jobs lost, and an additional 242,000 jobs shed across other industries such as retail, food service, and construction (George Washington University, 2025). The reduction in federal Medicaid funding, resulting from decreased enrollment, creates a ripple effect throughout state economies: healthcare providers are forced to cut staff and services, vendors lose business, and various industries experience job losses (George Washington University, 2025; National Health Law Program, 2025). As incomes decline, consumer spending decreases, tax revenues drop, and public budgets come under strain (George Washington University, 2025; National Health Law Program, 2025). In contrast, Medicaid expansion has been shown to stimulate job creation and economic activity, with Colorado, for example, gaining 31,074 new jobs and $3.8 billion in economic activity (Colorado Health Foundation, 2016). Conversely, work requirements could destabilize the low-wage workforce (National Health Law Program, 2025). This demonstrates a counterproductive economic impact. Instead of boosting employment, the policy causes significant job losses and reduces state GDP. The supposed "savings" at the federal level are offset by broader economic contraction at the state and local levels, including reduced tax revenues. This implies that a policy intended to save money and encourage work actually creates economic instability, increases unemployment, and strains state budgets, ultimately undermining overall economic health.
Challenges for Managed Care Organizations and Communication Barriers
The implementation of new work requirements also poses significant operational challenges for managed care organizations (MCOs), which serve approximately 80% of Medicaid expansion enrollees (Health Management, 2025a; Health Management, 2025b). These requirements make it more difficult for current Medicaid enrollees to maintain their insurance coverage (Fierce Healthcare, 2025). MCOs face substantial hurdles due to outdated regulations, specifically the 1991 Telephone Consumer Protection Act (TCPA), which severely restricts their ability to text members without explicit permission (Fierce Healthcare, 2025). This "outdated" texting ban renders modern communication "staggeringly inconvenient and unrealistic" for health plans attempting to send crucial updates like appointment reminders (Fierce Healthcare, 2025). The resulting low opt-in rates, such as the mere 3% in Virginia for state program messages, significantly hinder effective communication (Fierce Healthcare, 2025). The reliance on traditional mail or fax for communication is particularly problematic for low-income Medicaid members who may possess a phone but lack easy access to a computer or reliable internet for online portals (Fierce Healthcare, 2025). This highlights the digital divide as a barrier to care and compliance. The communication barrier, exacerbated by the digital divide, becomes another layer of "red tape" that disproportionately impacts vulnerable populations, making compliance with work requirements even harder. This systemic communication failure undermines care coordination, increases administrative burden for MCOs, and ultimately contributes to the cycle of coverage loss and increased reliance on acute care, despite the MCOs' efforts to manage care effectively. It underscores a policy contradiction where the government imposes complex requirements but hinders efficient communication tools necessary to meet them.
Furthermore, work requirements can significantly disrupt MCO risk pool stability and care coordination efforts (Health Management, 2025a; Health Management, 2025b). States must review existing vendor contracts and assess the need for new services, roles, and third-party reporting mechanisms to adapt to these changes (Health Management, 2025a; Health Management, 2025b). Lessons learned from the Medicaid unwinding following the COVID-19 public health emergency underscored the complexities of Medicaid systems, patient engagement, and the necessity of reliable member outreach methods (Health Management, 2025b). This creates systemic instability in managed care. The unpredictable and significant disenrollment caused by work requirements, particularly among vulnerable populations, destabilizes MCO risk pools, making it challenging for them to accurately predict and manage healthcare costs for their enrolled populations. This also severely disrupts continuity of care and care coordination efforts (Health Management, 2025a; Health Management, 2025b). The MCO model, designed to manage care and costs over time, is undermined by policies that introduce extreme instability in enrollment. This could lead to MCOs withdrawing from Medicaid programs or increasing their rates, further straining state budgets. This creates a fragmented and inefficient healthcare system where long-term health management is sacrificed for short-term "savings" from disenrollment. It highlights how policy changes can have unintended, detrimental effects on the operational stability of key healthcare delivery mechanisms.
Conclusion: A Policy with Proven Harms, Not Benefits
A thorough synthesis of the available evidence unequivocally demonstrates that Medicaid work requirements fail to achieve their stated goals and, instead, generate a cascade of negative health, social, and economic consequences. Overwhelming evidence from past implementations in Arkansas and Georgia, coupled with analyses from reputable organizations such as the CBO, Urban Institute, Commonwealth Fund, and KFF, consistently shows that these policies do not increase employment (ACLU, 2025; Brookings, 2025a; Center on Budget and Policy Priorities, 2025a; Commonwealth Fund, 2018; Commonwealth Fund, 2025b; National Health Law Program, 2025; Robert Wood Johnson Foundation, 2025; Urban Institute, 2025). Rather, they lead to massive coverage losses, primarily driven by administrative hurdles and "red tape," affecting millions of otherwise eligible individuals, including those who are already working or should qualify for exemptions (ACLU, 2025; Center on Budget and Policy Priorities, 2025a; Center on Budget and Policy Priorities, 2025b; Commonwealth Fund, 2025a; Commonwealth Fund, 2025b; Georgians for a Healthy Future, 2025; National Association of Community Health Centers, n.d.; Robert Wood Johnson Foundation, 2025).
These coverage losses disproportionately impact the most vulnerable populations, including people with disabilities, caregivers, individuals with chronic conditions, and children (ACLU, 2025; Bazelon Center for Mental Health Law, 2025; Center for American Progress, 2025; Center on Budget and Policy Priorities, 2025b; Commonwealth Fund, 2025d; KFF, 2025; Robert Wood Johnson Foundation, 2025). The implementation of these policies incurs high administrative costs, often diverting significant funds away from direct healthcare services (Bazelon Center for Mental Health Law, 2025; Milbank Memorial Fund, 2025; ProPublica and The Current, 2024; Robert Wood Johnson Foundation, 2025). Crucially, coverage disruptions lead to increased reliance on emergency departments, delayed necessary care, and a worsening of health outcomes, ultimately inflating overall healthcare costs through increased uncompensated care and the need for more intensive, acute interventions (ASPE, n.d.; America's Essential Hospitals, 2025a; America's Essential Hospitals, 2025b; Bazelon Center for Mental Health Law, 2025; Commonwealth Fund, 2025e; Commonwealth Fund, 2025f; National Health Law Program, 2025; Texas Health and Human Services, 2024; Texas Health and Human Services, 2025). The economic ripple effects are equally concerning, including significant job losses and reduced state GDP, demonstrating a counterproductive impact on state economies (Center for American Progress, 2025; George Washington University, 2025; National Health Law Program, 2025). This comprehensive analysis reveals the policy as a net negative for public health and economic stability. It is not merely ineffective; it is actively harmful, shifting burdens rather than creating efficiencies or promoting well-being.
Given the overwhelming evidence of their detrimental effects, continuing to pursue such policies indicates a prioritization of ideological positions or short-term budget cuts over evidence-based policymaking, public health, and the welfare of vulnerable citizens. Policymakers should instead prioritize strategies that genuinely support health and economic stability, such as investments in job training, affordable childcare, reliable transportation, and robust healthcare access, rather than imposing punitive measures that exacerbate existing disparities (Commonwealth Fund, 2025b; Commonwealth Fund, 2018). The insights gleaned from studies on "Contemporary Perspectives on Poverty" (OJIN, 2024a) and "Addressing Social Determinants of Health" (OJIN, 2025a) underscore the imperative to address the root causes of health disparities and poverty, rather than erecting barriers to care. Furthermore, embracing effective communication strategies, including modern digital tools, is essential for maintaining coverage and improving health outcomes, highlighting the urgent need to update outdated regulations that impede such efforts (Fierce Healthcare, 2025).
References
ACLU. (2025, March 28). Medicaid work requirements don't work — They harm people with disabilities. Retrieved from https://www.aclu.org/news/disability-rights/medicaid-work-requirements-dont-work-they-harm-people-with-disabilities
America's Essential Hospitals. (2025a, June). Estimated effects of H.R. 1 on hospital uncompensated care costs. Retrieved from https://essentialhospitals.org/wp-content/uploads/2025/06/CBO-Analysis-Reconciliation-June-2025.pdf
America's Essential Hospitals. (2025b). Estimated effects of H.R. 1 on hospital uncompensated care costs. Retrieved from https://essentialhospitals.org/estimated-effects-of-h-r-1-on-hospital-uncompensated-care-costs/
ASPE. (n.d.). Medicaid churning: A review of the evidence. U.S. Department of Health & Human Services. Retrieved from https://aspe.hhs.gov/sites/default/files/private/pdf/265366/medicaid-churning-ib.pdf
Ballotpedia. (n.d.). Medicaid work requirements in the states. Retrieved from https://ballotpedia.org/Medicaid_work_requirements_in_the_states
Bazelon Center for Mental Health Law. (2025, March 28). Medicaid work requirements don't work — They harm people with disabilities. Retrieved from https://www.bazelon.org/wp-content/uploads/2025/03/3-28-25-Bazelon-Resource-on-Medicaid-Work-Requirements-final.pdf
Brookings. (2025a, May 22). How proposed changes to Medicaid are expected to impact near-elderly Americans. Retrieved from https://www.brookings.edu/articles/how-proposed-changes-to-medicaid-are-expected-to-impact-near-elderly-americans/
Brookings. (2025b, May 22). Any way you look at it you lose: Medicaid work requirements will either fall short of anticipating savings or harm vulnerable beneficiaries. Retrieved from https://www.brookings.edu/articles/any-way-you-look-at-it-you-lose-medicaid-work-requirements-will-either-fall-short-of-anticipating-savings-or-harm-vulnerable-beneficiaries/
CBS News. (2025, May 22). Republicans weigh Medicaid requirements, Georgia's experience offers a warning. Retrieved from https://www.cbsnews.com/news/medicaid-bill-work-requirement-funding-cuts-what-to-know/
Center for American Progress. (2025, May 24). The collateral damage of Medicaid work requirements. Retrieved from https://www.americanprogress.org/article/the-collateral-damage-of-medicaid-work-requirements/
Center on Budget and Policy Priorities. (2025a, May 22). Harsh work requirements in House Republican bill would take away Medicaid coverage from millions: State and congressional district estimates. Retrieved from https://www.cbpp.org/research/health/harsh-work-requirements-in-house-republican-bill-would-take-away-medicaid-coverage
Center on Budget and Policy Priorities. (2025b, May 22). Medicaid work requirements will reduce low-income families’ access to care and worsen health outcomes. Retrieved from https://www.cbpp.org/research/health/medicaid-work-requirements-will-reduce-low-income-families-access-to-care-and-worsen
Colorado Health Foundation. (2016, June). Assessing the economic and budgetary impact of Medicaid expansion in Colorado: FY 2015-16 through FY 2034-35. Retrieved from https://shvs.org/medicaid-expansion-resource-center/
Commonwealth Fund. (2018, November). Medicaid work requirements: Will they help the unemployed gain jobs or improve health? Retrieved from https://www.commonwealthfund.org/sites/default/files/2018-11/Ku_Medicaid_work_requirements_ib.pdf
Commonwealth Fund. (2025a, January 14). Work requirements for Medicaid enrollees. Retrieved from https://www.commonwealthfund.org/publications/explainer/2025/jan/work-requirements-for-medicaid-enrollees
Commonwealth Fund. (2025b, May). Medicaid work requirements: Job losses harm states. Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2025/may/medicaid-work-requirements-job-losses-harm-states
Commonwealth Fund. (2025c, May). Medicaid work requirements: Job losses harm states. Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2025/may/medicaid-work-requirements-job-losses-harm-states
Commonwealth Fund. (2025d, May 30). Nearly 5.6 million community health center patients could lose Medicaid coverage under new work requirements, with revenue losses up to $32 billion. Retrieved from https://www.commonwealthfund.org/blog/2025/community-health-center-patients-medicaid-coverage-work-requirements
Commonwealth Fund. (2025e, May). Federal cuts to Medicaid could end Medicaid expansion and affect hospitals. Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2025/may/federal-cuts-medicaid-could-end-medicaid-expansion-affect-hospitals
Commonwealth Fund. (2025f, May). Federal cuts to Medicaid could end Medicaid expansion and affect hospitals. Retrieved from https://www.commonwealthfund.org/publications/issue-briefs/2025/may/federal-cuts-medicaid-could-end-medicaid-expansion-affect-hospitals
Fierce Healthcare. (2025, June 4). Medicaid work requirements: Trump bill revives calls to update managed care texting ban. Retrieved from https://www.fiercehealthcare.com/payers/medicaid-work-requirements-trump-bill-revives-calls-update-managed-care-texting-ban
George Washington University. (2025, May 1). New state-by-state report: Medicaid work requirements threaten up to half a million jobs and could drain state economies by $59 billion in 2026 alone. Retrieved from https://publichealth.gwu.edu/new-state-state-report-medicaid-work-requirements-threaten-half-million-jobs-and-could-drain-state
Georgians for a Healthy Future. (2025, May 22). Public has until June 1 to comment on Georgia's Medicaid work requirements as coverage barriers persist. Retrieved from https://gbpi.org/public-has-until-june-1-to-comment-on-georgias-medicaid-work-requirements-as-coverage-barriers-persist/
Gustin, T., Parrott, J., McCasland, J., & Rutledge, C. (2024, June 30). Academic practice partnerships: Improving healthcare access and decreasing system burden utilizing interprofessional competencies. The Online Journal of Issues in Nursing, 29(3). https://ojin.nursingworld.org/table-of-contents/volume-29-2024/number-3-september-2024/articles-on-previously-published-topics/academic-practice-partnerships/
Health Management. (2025a, May 22). Evolving Medicaid work requirement policies: Essential state actions to prepare. Retrieved from https://www.healthmanagement.com/blog/evolving-medicaid-work-requirement-policies-essential-state-actions-to-prepare/
Health Management. (2025b, May 22). Building state capacities for Medicaid work and community engagement requirements. Retrieved from https://www.healthmanagement.com/blog/building-state-capacities-for-medicaid-work-and-community-engagement-requirements/
KFF. (2025, May 22). Tracking the Medicaid provisions in the 2025 budget bill. Retrieved from https://www.kff.org/tracking-the-medicaid-provisions-in-the-2025-budget-bill/
Milbank Memorial Fund. (2025, June 1). Lessons learned from Arkansas' experience with a Medicaid work requirement. Retrieved from https://www.milbank.org/2025/06/lessons-learned-from-arkansas-experience-with-a-medicaid-work-requirement/
National Association of Community Health Centers. (n.d.). Harmful impacts of Medicaid work requirements. Retrieved from https://www.nachc.org/harmful-impacts-of-medicaid-work-requirements/
National Health Law Program. (2025, March). Medicaid work requirements would gut state and local economies. Retrieved from https://healthlaw.org/wp-content/uploads/2025/03/Medicaid-Work-Requirements-Would-Gut-State-and-Local-Economies_Morcelle.pdf
OJIN. (2024a, January 31). Contemporary perspectives on poverty. The Online Journal of Issues in Nursing. Retrieved from https://ojin.nursingworld.org/topics/contemporary-perspectives-on-poverty/
OJIN. (2025a, May). Addressing social determinants of health: Progress and opportunities. The Online Journal of Issues in Nursing. Retrieved from https://ojin.nursingworld.org/topics/social-determinants-of-health/
ProPublica and The Current. (2024, December 12). Republicans weigh Medicaid requirements, Georgia's experience offers a warning. Yahoo News. Retrieved from https://www.yahoo.com/news/republicans-weigh-medicaid-requirements-georgia-124000041.html
Robert Wood Johnson Foundation. (2025, April 24). Work requirements threaten health and increase costs. Retrieved from https://www.rwjf.org/en/insights/our-research/2025/04/work-requirements-threaten-health-and-increase-costs.html
Texas Health and Human Services. (2024, March). Biannual report on initiatives to reduce avoidable emergency room utilization and improve health outcomes in Medicaid. Retrieved from https://www.hhs.texas.gov/sites/default/files/documents/initiatives-reduce-avoidable-er-utilization-improve-health-outcomes-medicaid-march-2024.pdf
Texas Health and Human Services. (2025, March). Biannual report on initiatives to reduce avoidable emergency room utilization and improve health outcomes in Medicaid. Retrieved from https://www.hhs.texas.gov/sites/default/files/documents/initiatives-reduce-avoidable-er-utilization-improve-health-outcomes-medicaid-march-2025.pdf
Tradeoffs. (2025, April 24). Medicaid work requirements are back. What you need to know. Retrieved from https://tradeoffs.org/2025/04/24/medicaid-work-requirements-are-back-what-you-need-to-know/
Urban Institute. (2025, February 28). New evidence confirms Arkansas's Medicaid work requirement did not boost employment. Retrieved from https://www.urban.org/urban-wire/new-evidence-confirms-arkansas-medicaid-work-requirement-did-not-boost-employment